3 min read
Value Based Reimbursement: The Evolution of Quality and Patient Safety
Performance Health Partners
March 5, 2023
Healthcare reimbursement describes the payment that a hospital, diagnostic facility, or other healthcare provider receives for providing patients with a medical service. This model has undergone significant changes over time, now incorporating value based reimbursement systems as a primary means of payment. It’s important to look at how the healthcare reimbursement model has changed over time in order to understand the processes underlying the current U.S. healthcare system, as well as the gaps and limitations that exist within it.
The Importance of Quality in Healthcare: Value Based Care Model
Following the passage of the Affordable Care Act in 2010, reimbursements became heavily tied to patient satisfaction and the quality of care provided—not the quantity.
The Affordable Care Act established the Hospital Value-Based Purchasing (VBP) Program, which is a Centers for Medicare & Medicaid Services (CMS) initiative that “rewards acute-care hospitals with incentive payments for the quality of care provided”.
With the shift towards value based reimbursement, hospitals are no longer paid solely on the quantity of services provided. Instead, CMS rewards hospitals based on:
- The quality of care provided to patients
- How closely best practices are followed
- How well hospitals enhance patients’ experiences of care during hospital stays
In practice, this means that reimbursement is tied to outcomes.
Early History of Healthcare Reimbursement
From 1920 to 1930, healthcare costs began to rise as people moved from rural to urban areas and treatment of acute illnesses moved from family homes to hospitals. During this time period, Blue Cross and Blue Shield came into existence.
A group of school teachers in Dallas, Texas “contracted with Baylor Hospital to provide 21 days of hospitalization for $6 per year”, which eventually became the inspiration for Blue Cross. The Blue Cross plan allowed open access to quality hospitals. An insurance plan for physician services known as Blue Shield came along in the 1930s.
The health insurance industry grew from the 1940s through the 1960s as medical technology evolved and as the government encouraged the practice of including health insurance as part of employee compensation packages. During that time, employers did not have to pay payroll tax on their contributions to employee health plans and employees did not have to pay income tax contributions to their health insurance plans paid by their employers.
In 1965, Medicare was put into place as a federal program with uniform standards of Parts A and B.
Part A consisted of the compulsory hospital insurance program where people were automatically enrolled at age 65. Part B served as a supplemental medical insurance for physicians’ services.
At that time, physicians stood to benefit from Medicare by billing patients directly for a reasonable rate and then the patient was reimbursed by Medicare.
Providing Quality Healthcare
The Health Maintenance Organization (HMO) Act of 1973 was enacted with the intention of containing costs and providing healthcare quality for populations that were previously underserved.
Fee-for-service medicine had led to health care inflation because it encouraged caregivers to maximize the number of procedures they perform, ignoring preventive care. Doctors and hospitals were not paid to keep patients well; they were paid to treat them when they were sick.
Unfortunately, the HMO era did not result in significant greater value for the price of healthcare.
The Movement Towards Quality Measures
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) was enacted to improve payments to physicians and other clinicians while rewarding value and outcomes via a Quality Payment Program. Eligible clinicians can participate as an individual or a group in one of two tracks: a. Merit-based Incentive Payment System (MIPS) or b. Advanced Alternative Payment Models (Advanced APMs). (See MIPS Graph 1).
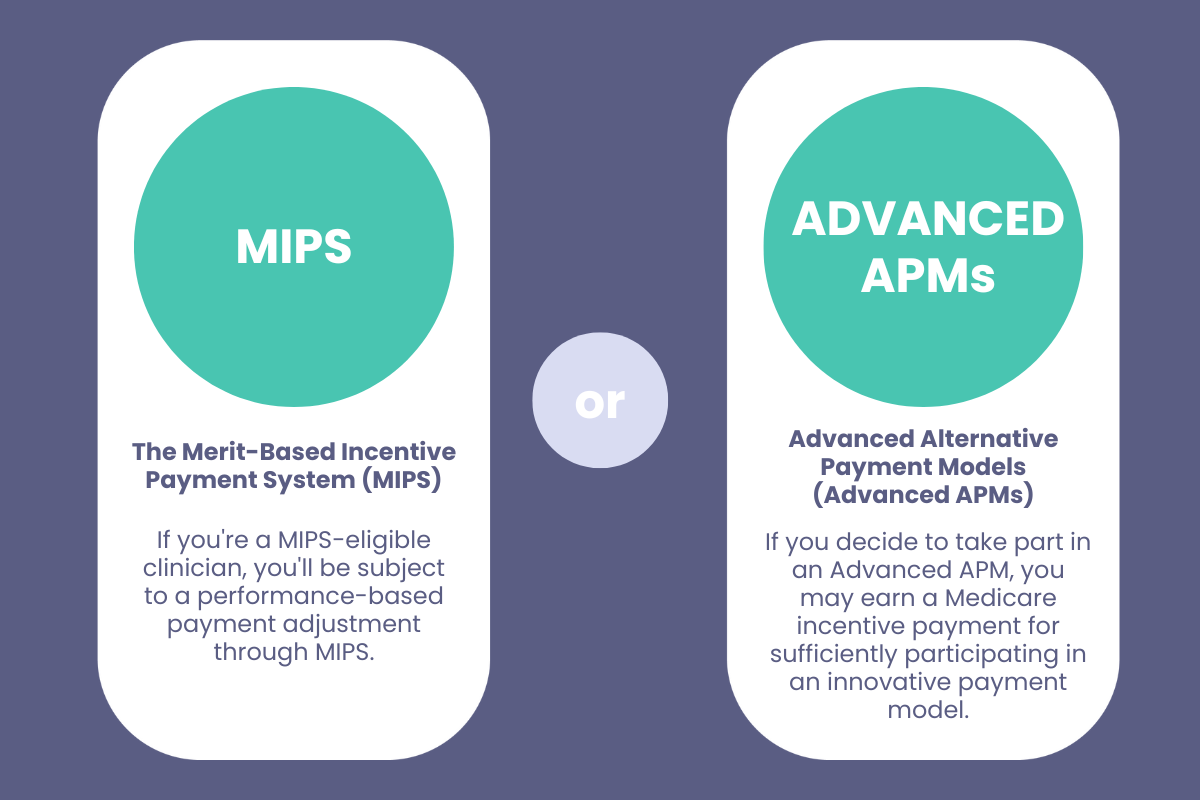 MIPS Graph 1
MIPS Graph 1
Clinicians are expected to actively measure and report their quality measures. It is important to note that there are more than 250 quality measures in MIPS.
Clinicians may report on “at least six quality measures, including at least one outcome measure or a high priority measure”.
The six domains for MIPS quality measures include:
-
- Patient safety
- Person and caregiver-centered experience and outcomes
- Communication and care coordination
- Effective clinical care
- Community/population health
- Efficiency and cost reduction
Once all data is submitted, Medicare payments are adjusted for eligible clinicians based on their MIPS Final Score.
High-Quality Care Over Quantity of Care
As healthcare costs and forms of reimbursement have evolved over time, so have the models of care used by healthcare organizations. With the movement towards value based reimbursement, organizations are now rewarded for providing high-quality care over quantity. This transition has driven organizations to achieve higher levels of patient safety and quality monitoring so that they can not only maximize reimbursement and maintain fiscal stability, but improve their outcomes in value-based care.
Benefits of Value Based Care: Software Solution for Healthcare
One way to achieve higher quality care outcomes is to implement a software solution for quality, incident reporting, and performance improvement. Benefits of implementing a software solution include:
- Streamlined reporting
- Customized dashboards and analytics
- Central channel for team communication
- Secure document storage
- Real-time notifications and alerts
- Workflows and follow-up management
To learn more about the value based reimbursement model and implementing software solutions to improve healthcare outcomes, request a demo here:

