
Measuring and tracking patient safety events can have a meaningful impact in making care safer and reducing costs through the prevention of healthcare-acquired conditions (HACs).
While HACs can cause both patient harm and substantial financial burden to an organization, many HACs are preventable with the implementation of patient safety and clinical quality technology that strengthens care delivery and drives quality outcomes.
Calculating the Cost of HACs
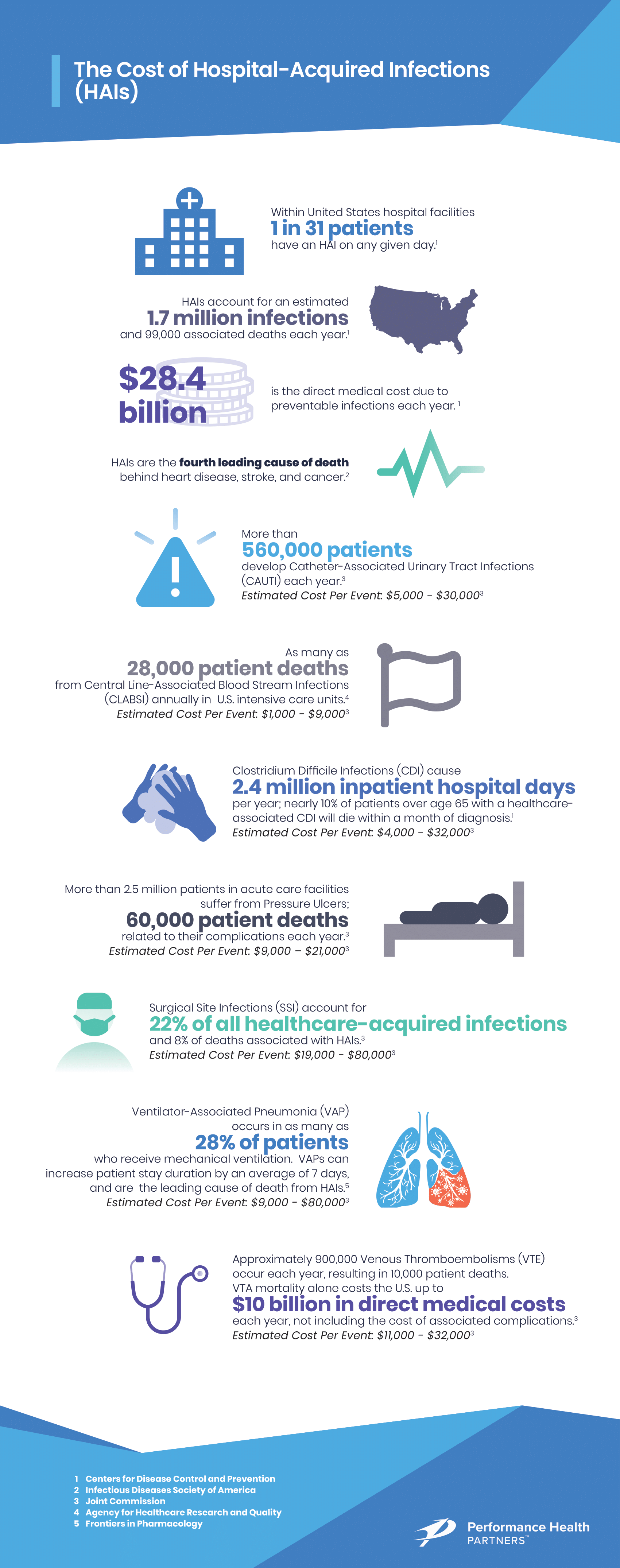
As detailed below, prevention of patient safety events like healthcare-acquired infections can yield substantial cost savings, reduce patient stay durations, markedly improve patient outcomes, and save lives. (1)
According to the Agency for Healthcare Research and Quality, patient safety events like HACs commonly impact healthcare organizations in the following ways:
Adverse Drug Events (ADE)
Estimated Cost Per Incident: $1,000-$9,000 (1)
Improper medication reconciliation, or medication discrepancies, account for roughly one of every three adverse events in healthcare facilities, affect nearly two million patients each year, and prolong a patient’s stay by 1.7 to 4.6 days. (3)
Catheter-Associated Urinary Tract Infections (CAUTI)
Estimated Cost Per Event: $5,000–$30,000 (1)
CAUTI’s are the most commonly reported HAC. More than 560,000 patients develop a CAUTI each year, and rates are on the rise. CAUTI’s are known to extend patient stays, increase costs, and contribute to patient morbidity and mortality. (4)
Central Line-Associated Blood Stream Infections (CLABSI)
Estimated Cost Per Event: $18,000–$95,000 (1)
CLABSI’s are associated with significant increases in patient morbidity, mortality, and costs—it is estimated that as many as 28,000 patients die from CLABSI annually in U.S. intensive care units. (5)
Clostridium Difficile (C. diff) Infections (CDI)
Estimated Cost Per Event: $4,000–$32,000 (1)
C-diff—a bacterium that causes diarrhea and colitis—is estimated to cause nearly half a million illnesses in the U.S. each year. Roughly 20% of patients who get C. diff will get it again, and nearly 10% of patients over age 65 with a healthcare-associated C. diff infection will die within a month of diagnosis. (6) The cost of this is staggering—the infection causes 2.4 million inpatient hospital days per year and adds $1.5B to annual healthcare costs. (7)
Falls
Estimated Cost Per Event: $3,000–$15,000 (1)
In 2018, the number one sentinel event in health care facilities was falls with injury. (8) Each year, 700,000-1,000,000 people in the United States fall in a healthcare facility (9), and roughly 25% of them will suffer a fall-related injury, resulting in increased healthcare utilization, the longer patient stays, higher costs, and greater liability. Patients who have a serious injury related to a fall while in a healthcare facility average 6–12 days of additional patient stay time than comparable patients who did not fall. (10)
Obstetric Adverse Events (OBAE)
Estimated Cost Per Event: Up to $1,000 (1)
Serious obstetrical adverse events—which include harm to either the mother or the infant—occur in approximately 9% of all U.S. births. (11)
Pressure Ulcers
Estimated Cost Per Event: $9,000–$21,000 (1)
Each year more than 2.5 million patients in U.S. acute care facilities suffer from pressure ulcers/injuries. These healthcare-acquired pressure ulcers/injuries cause roughly 60,000 patients to die from their complications each year. (12)
Surgical Site Infections (SSI)
Estimated Cost Per Event: $12,000–$42,000 (1)
SSIs are the second most common type of healthcare-acquired infection, accounting for 22% of all healthcare-acquired infections and 8% of deaths associated with healthcare-acquired infections. (13) SSI’s cost the U.S. healthcare system $3.5-$10 billion annually. (14)
Ventilator-Associated Pneumonia (VAP)
Estimated Cost Per Event: $19,000–$80,000 (1)
VAP is a complication that occurs in as many as 28% of patients who receive mechanical ventilation and is the leading cause of death from healthcare-acquired infection. VAP increases patient stay duration by an average of seven days. (15)
Venous Thromboembolism (VTE)
Estimated Cost Per Event: $11,000–$32,000 (1)
It is estimated that up to 900,000 VTEs occur each year in the U.S., resulting in approximately 100,000 patient deaths. VTE mortality alone costs the U.S. $8-$10 billion in direct medical costs each year, not including the costs of associated complications. (16)
How Implementing a Patient Safety Platform Impacts Outcomes
An incident reporting system is a critical component to improve quality, safety, and efficiency and reduce health disparities across healthcare organizations by allowing them to track and learn from patient safety incidents. An incident is an event or circumstance that could have resulted — or did result — in harm to a patient. (17)
Even “near misses”, or events that did not result in patient harm (but could have), provide opportunities for proactive learning and improvement. When healthcare organizations rely upon manual patient safety tracking, they risk inconsistent or incomplete data entry and lack the tools for effectively synthesizing event data for the purposes of learning, training, prompt remediation, and prevention.
Conclusion
Healthcare-acquired conditions and other patient safety events can be prevented through the effective implementation of patient safety programs. Patient safety programs help healthcare organizations streamline reporting and track data over time in order to identify areas of improvement, while also providing a significant cost avoidance opportunity.
References:1- Agency for Healthcare Research and Quality. (2016, December 9). AHRQ Tools To Reduce Hospital-Acquired Conditions. Retrieved from https://www.ahrq.gov/hai/hac/tools.html
2- Agency for Healthcare Research and Quality. (2019, January 29). AHRQ Analysis Finds Hospital-Acquired Conditions Declined By Nearly 1 Million from 2014-2017. Retrieved from https://www.ahrq.gov/news/newsroom/press-releases/hac-rates-declined.html
3- Office of Disease Prevention and Health Promotion. (2019, September 24). Overview. Retrieved from https://health.gov/hcq/ade.asp
4- American Nurses Association. (n.d.). ANA CAUTI Prevention Tool. Retrieved from https://www.nursingworld.org/practice-policy/work-environment/health-safety/ infection-prevention/ana-cauti-prevention-tool/
5-Agency for Healthcare Research and Quality. (2018, July 25). Central Line-Associated Bloodstream Infections (CLABSI). Retrieved from https://www.ahrq.gov/ topics/central-line-associated-bloodstream-infections-clabsi.html
6-Centers for Disease Control and Prevention. (2018, December 17). What is C. diff? Retrieved from https://www.cdc.gov/cdiff/what-is.html#anchor_1540390280946
7-Joint Commission Center for Transforming Healthcare. (2015). Reducing C. Diff Infections. Retrieved from https://www.centerfortransforminghealthcare.org/ improvement-topics/reducing-c-diff-infections
8- Patient Safety & Quality Healthcare. (2018, December 19. TJC Releases Compliance and Sentinel Event Stats for First Half of 2018. Retrieved from https://www. psqh.com/analysis/tjc-releases-compliance-and-sentinel-event-stats-for-first-half-of-2018/
9- Agency for Healthcare Research and Quality. (2013, January 31). Preventing Falls in Hospitals. Retrieved from https://www.ahrq.gov/professionals/systems/ hospital/fallpxtoolkit/index.html
10- Bouldin, E. L. D., Andresen, E. M., Dunton, N. E., Simon, M., Waters, T. M., Liu, M., … Shorr, R. I. (2013, March). Falls among adult patients hospitalized in the United States: prevalence and trends. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3572247/
11- RTI International. (2016, November 17). Safety Program for Perinatal Care. Retrieved from https://www.rti.org/impact/safety-program-perinatal-care
12- Joint Commission Center for Transforming Healthcare. (2017). Hospital Acquired Pressure Ulcers Prevention. Retrieved from https://www.centerfortransforminghealthcare.org/en/improvement-topics/hospital-acquired-pressure-ulcers-prevention
13- Joint Commission Center for Transforming Healthcare. (2019). Surgical Site Infections. Retrieved from https://www.centerfortransforminghealthcare.org/ improvement-topics/surgical-site-infections
14- https://www.journalofhospitalinfection.com/article/S0195-6701(17)30135-4/pdf#:~:text=Alfonso%20et%20al.%20reported%20that,%25%20and%206%25%2C%20respectively.
15- Timsit, J.-F., Esaied, W., Neuville, M., Bouadma, L., & Mourvllier, B. (2017, November 29). Update on ventilator-associated pneumonia. Retrieved from https://www. ncbi.nlm.nih.gov/pmc/articles/PMC5710313
16- Joint Commission Center for Transforming Healthcare. (2018). Venous Thromboembolism (VTE) Prevention. Retrieved from https://www.centerfortransforminghealthcare.org/improvement-topics/venous-thromboembolism-prevention



