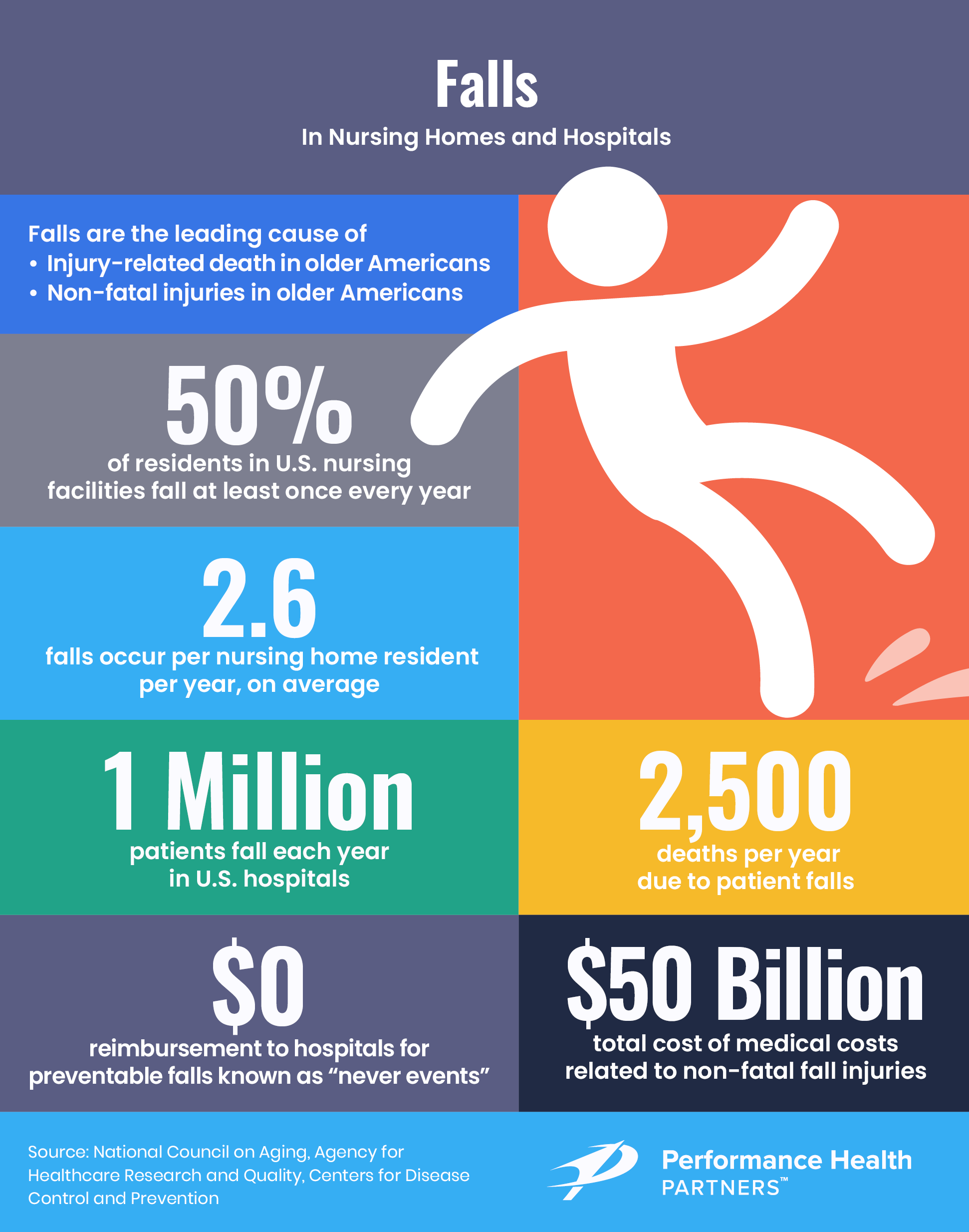
Every second of every day, an older adult over the age of 65 suffers a fall in the United States. Furthermore, approximately 700,000 to 1,000,000 people fall in U.S. hospitals every year, according to the Agency for Healthcare Research and Quality. Patients aged 85 and older as well as those who have undergone recent surgery are more likely to be seriously injured if they fall.
Patient Falls in Healthcare
More than one-third of in-hospital falls result in injury, including serious injuries such as fractures and head trauma.
Falls among patients continue to be the most frequently reported sentinel event, accounting for 47% of all reports in the first half of 2023. The economic impact is also significant, with annual medical care costs related to falls estimated at around $50 billion.
Beyond the financial costs, the consequences of falls are severe for the patients themselves: injuries from falls can result in extended hospital stays—up to 12 additional treatment days—as well as the need for surgery or, in the worst cases, leading to fatalities.
Moreover, even in the absence of physical injuries, a fall can induce a fear of falling again, which often results in decreased mobility and a lack of confidence.
Quality improvement programs can drastically reduce fall risk in the hospital setting. The Mercy Health-Anderson Hospital medical/surgical unit in Cincinnati was able to reduce its fall rate from 10 patient falls per 1,000 patient days to two falls per 1,000 patient days over three years through a quality improvement program called Transforming Care at the Bedside, an initiative that focuses on improving care on medical and surgical units.
"The med/surg unit is kind of the unsung hero. It's the backbone of the hospital in many ways, but there's not always a lot of focus on [its] operations. The goals of the TCAB program were to transform leadership, retain and engage med/surg nurses, improve quality of care on med/surg units, make care more streamlined and efficient and improve the patient experience with a real focus on everything being patient centered."
- Terri Martin, RN, BSN, MBA, Clinical Director of Anderson Hospital and TCAB program leader.
These staggering numbers underscore the importance for a well-established fall prevention plan.
How to Prevent Patient Falls: 10 Effective Tips
Read on for 10 best practices for fall prevention strategies.
1. Assess each individual patients’ risk for falling
Fall risk screening should be conducted at every admission to determine which patients are considered high-risk for falling. Patient risk factors include:
-
- Illnesses that cause weakness
- Medicines that cause dizziness, including nonprescription medications
- Delirium
- New or unfamiliar environments
- Lack of activity
- Elderly age, especially those who are 85 and over
Another best practice is to use visual cues, such as red socks or color-coded armbands, to help staff recognize patients who have a high risk of falling at a quick glance. Through such visual cues, staff can quickly initiate the correct protocols and procedures to reduce fall risk. The American Hospital Association recommends that healthcare facilities standardize colors to avoid confusion, indicating yellow as the color for falls risk.
2. Implement and adhere to a mobility plan
Adhering to a well-defined mobility plan is essential for patient safety, promoting an active lifestyle that enhances strength and stability. Regular physical activity tailored to each patient's needs not only boosts their overall health but also significantly improves their balance and coordination, key factors in preventing falls.
When possible, patients should work closely with physiotherapists to engage in exercises designed specifically for their health condition and treatment plan. This frequent, guided physical activity ensures that movements are performed safely and effectively, maximizing the benefits of exercise while minimizing the risk of falls. By integrating structured mobility plans into patient care, healthcare providers can create a proactive approach to maintaining patient mobility and preventing injuries.
3. Ensure caregiver support during restroom visits
To effectively prevent falls, caregivers should be within arm's reach when patients attend the restroom, especially given that over 34% of patient falls occur in relation to toileting, with a significant 44% of these falls happening during the night.
Implementing a toileting schedule ensures that a staff member is always available to assist patients when they need to use the restroom. Additionally, equipping restrooms with grab bars provides essential support for patients as they sit down and stand up, further reducing the risk of falls.
This proactive approach not only safeguards patients but also builds a supportive environment that prioritizes their safety and dignity during vulnerable moments.
4. Provide safe footwear rather than just advising it
Rather than merely advising patients to wear safe footwear, healthcare facilities should take a proactive stance by providing easy access to non-skid footwear, such as rubber-soled slippers or socks with grips.
This is especially important for patients identified as prone to falling. By ensuring that all such patients have immediate access to appropriate footwear, facilities significantly enhance safety by reducing the risk of slips and falls.
5. Use bed alarms
Bed alarms can be used to alert staff whenever a patient at high risk for falls leaves their bed. Healthcare workers must be responsive to alarms for these devices to be effective. An alarm should be used only if it makes sense for the individual patient to avoid unnecessary errors.
If used, the bed alarm's time interval should be no more than one or two seconds between the time a patient leaves the bed and the time the alarm sounds — otherwise, the patient could be halfway down the hall before it rings.
6. Conduct regular safety rounding
One of the most effective strategies to prevent falls is conducting safety rounds on high fall-risk patients in addition to regular hourly rounds. During the safety rounds, a staff member should attend to basic needs such as assessing the patient’s pain, bed position, and need to visit the restroom. Staff should also make sure that all precautions to prevent falls are in place, that the environment is uncluttered and assistive devices are within reach.
7. Review and/or discontinue medications associated with a high risk of falls
Psychoactive medications such as benzodiazepines can increase a patient’s risk of falls by nearly 47%. It is important that healthcare providers routinely review medication side effects and work with pharmacists to develop a management plan to reduce fall risk, especially in older adults.
8. Provide easy access to mobility aids
To minimize the risk of falls, it's crucial that mobility aids like canes and wheeled walkers are easily accessible to patients who demonstrate a need for them. A simple way to assess this need is to observe whether a patient reaches for support while walking.
Providing these aids promptly can significantly enhance a patient's stability and confidence, reducing the likelihood of falls. Storing these tools in consistent, familiar locations and ensuring they are well-maintained tailors the environment to support patient safety effectively.
9. Engage patients with activity
Giving patients different activities to do helps them stay occupied and are therefore less likely to get out of bed. Staff can encourage patients to practice exercises that they can do while lying in the hospital bed. These activities offer dual benefits: they maintain mental engagement and build physical strength, both of which are crucial in reducing fall risk.
By actively involving patients in their own care through these safe exercises, we not only enhance their well-being but also foster an environment that prioritizes fall prevention.
10. Implement a risk management system for safety rounds
A risk management system can help care providers document previous fall history and assess this information to define departmental areas of improvement. Rounding tools and incident reporting software make it simple for staff members to proactively address patient needs and environmental concerns and correct any deficiencies prior to a fall occurring.
Technology to Prevent Patient Falls
Performance Health Partners helps healthcare organizations provide the highest quality care in the safest possible environment using technology to prevent patient falls.
Learn how incident reporting systems help care teams proactively identify falls and other patient safety risks to get ahead of incidents before they happen.