4 min read
Value Based Care: Using Access Centers to Improve Outcomes
Performance Health Partners
April 21, 2020

As the healthcare industry moves towards a value based care reimbursement model, it becomes increasingly important for healthcare organizations to effectively manage costs and improve their margins. Access centers address these challenges.
Access Centers: The Need and The Challenges
Healthcare systems are increasingly focused on improving patient access to care in order to attract new patients and retain existing ones. (1)
Access centers act as an entry point to health systems and are critically important in not only improving patient outcomes, but also expanding revenue and improving margins. (1)
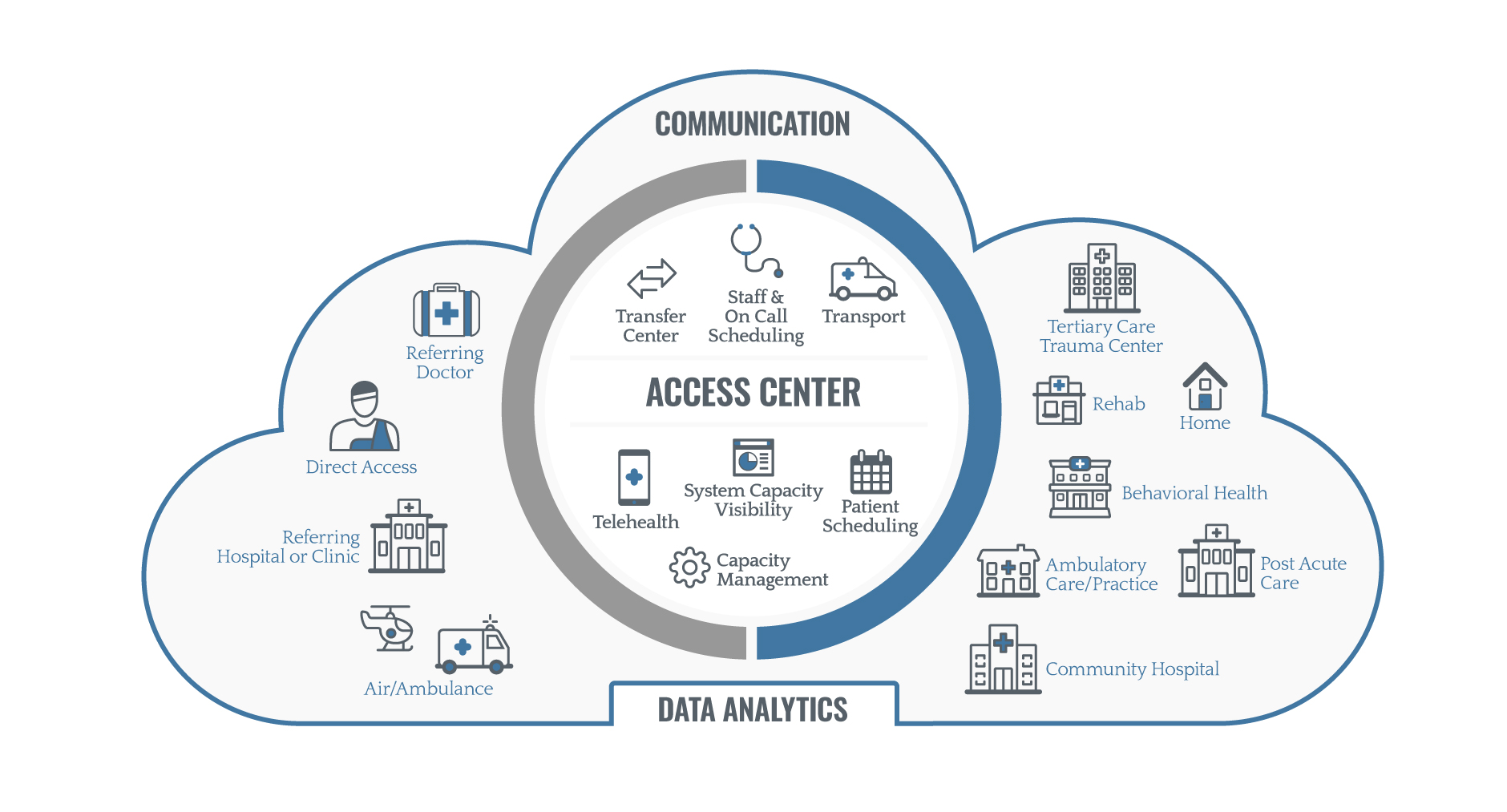
Common types of access centers include emergency departments, ambulance services, referring hospitals or clinics, and telehealth. (2)
Access centers act as liaison between inpatient and outpatient centers and are responsible for coordinating the handoff of the patient as efficiently as possible (2). Successful access centers combine many elements, such as patient scheduling, communication tools, and purpose-built platforms for tracking data and analytics in order to efficiently connect patients to care.
Roles of the Access Center
As access centers evolve with the healthcare industry, systems are becoming increasingly complex and difficult to navigate and access — both for patients and providers. (2)
What used to be inbound and outbound movement in transfer centers is now evolving into a more dynamic, centralized access center model.
The access center serves as a central point for all types of care, including telehealth, home health, behavioral health, post-acute care, and more. (2)
Roles of the access center include (2):
- Interfacility transfers
- Direct referrals & admissions
- Capacity, placement
- Telehealth
- Staff coordination
- Transport
- Patient scheduling
- Data and analytics
Value Based Reimbursement: Expanding Revenue & Improving Margins
As the healthcare industry moves towards a value based care reimbursement model, it becomes increasingly important for healthcare organizations to effectively manage costs and improve their margins.
According to Beckers Healthcare,
“Working in healthcare, we’re first and foremost always focused on patient care. But we’re also running a business. And we should all recognize that running a strong business with strong revenue helps us better achieve our mission.” (2)
Particularly in rural hospitals, Becker’s Healthcare notes, “if there’s no margin, there’s no mission. No one is immune to looking at the business side of how a hospital or healthcare system is run, to be able to achieve their mission.” (2)
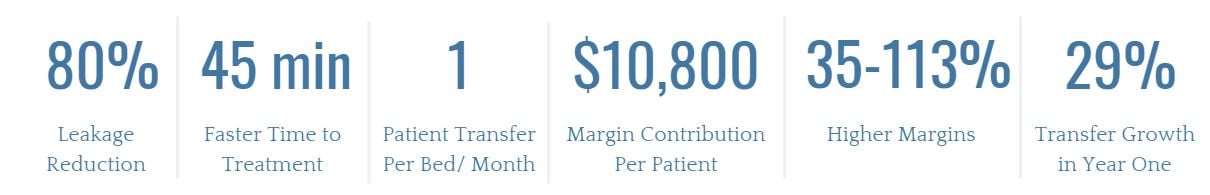
Highly effective access center models drive rapid acceptance rates and deliver patients to care at a much faster rate than the traditional EMS model. (2) According to a recent study, a well-run access center can result in (2):
Value Based Care: Common Challenges
There are several common challenges faced by healthcare executives as they attempt to navigate value-based care models and implement successful access centers (3):
1. Financial challenges due to leakage
Many healthcare departments are “leaking out” patients to competitors in high volumes.
Some, such as emergency departments, are suffering up to 80% leakage for the services that they provide. (2)
A well-run access center keeps those patients within network and provides much faster treatment times from diagnosis to definitive treatment.
2. Inconsistent processes
Healthcare facilities often struggle with inconsistent processes for patient transfers and access. For example, according to a study on one hospital, “prior to the development of an access center, referring physicians would either attempt to call an accepting physician specialist or contact personnel in the emergency room.
The emergency room personnel would then contact an accepting specialist, who would call the nurse supervisor, who would call bed control to ensure bed availability. This inconsistent process was cumbersome and frequently led to loss of referrals.” (4)
3. Lack of communication between organizations and within departments
Poor communication has been a factor in 1,744 patient deaths and over $1.7 billion in malpractice costs nationally in the past five years, according to a report by CRICO Strategies. (5)
4. Poor patient experience
The patient experience starts when a patient calls an access center and speaks with an agent, which begins the patient-provider matching process. (1) The effectiveness of service in the access center has a direct impact on patient satisfaction scores; if patients have a negative experience starting at the access center, it sets the tone for the patient’s relationship with the organization moving forward. (1)
5. Lack of data-driven platforms for patient safety and quality
Many healthcare organizations rely on paper methods or solutions created in-house to track patient safety and quality. However, those methods often lack the robust technology, data and analytics needed to identify trends over time and improve outcomes.
Overcoming Challenges with Purpose-Built Technology
How can healthcare organizations achieve the highest quality outcomes possible with value based care and access centers? A purpose-built technology platform gives care teams a single platform that provides a detailed, transparent look into what’s going on in the market globally. (2)
Performance Health Partner's technology solutions help healthcare organizations overcome common challenges and provides the following benefits:
1. Track transfers with real-time dashboards
A technology platform can help care teams track transfers in and out of an organization. Real-time dashboards help identify trends and recognize patients who are at risk of seeking care at another facility.
2. Consistency in processes
Technology platforms streamline processes through automatic workflows and notifications, so all members of a care team remain up-to-date and on track with action plans. All processes are documented and easy to follow in the platform, ensuring consistency and maximum efficiency across departments.
3. Clear communication
A technology platform provides a centralized command center for team collaboration, action plans, and next steps. It removes silos and communication barriers by making sure that all staff members are on the same page, and that important information doesn't get lost in email threads or undocumented conversations.
4. Improve patient experience
Cultivating a positive patient experience with the help of a technology platform can go a long way in improving patient satisfaction. With an online platform, patients and their families can fill out patient feedback surveys that trigger corresponding action plans to guide staff through performance improvements.
5. Data-driven platforms inform decision making
Having clearly visible data in easily accessible forms such as custom dashboards allows healthcare executives to make better decisions more quickly, which improves patient outcomes and enhances margins. A technology platform can also integrate with other IT systems to make sure that all available data is easily accessible in one place.
As value based care and the role of the access center continues to evolve, healthcare executives and teams can turn to these practices in order to improve outcomes while expanding revenue.

References-
1- Five Things Health Systems Leaders Need to Know About Access Centers. August 2017. Retrieved at https://www.kyruus.com/blog/five-things-health-systems-leaders-need-to-know-about-access-centers
2- Beckers Healthcare Webinar. How better management of patient transfers can expand revenue, improve margins. March 23, 2020. Retrieved at https://event.on24.com/wcc/r/2229191/7F72EF5F4D983EB53409F6030D510E02.
3- Top Issues Confronting Hospitals. American College of Healthcare Executives. 2020. Retrieved at https://www.ache.org/learning-center/research/about-the-field/top-issues-confronting-hospitals/
4- The Development of the Patient Transfer Center at Ochsner Medical Center. The Ochsner Journal. 2009. Retrieved at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096277/
5- Medication-related Malpractice Risks. CRICO Strategies. 2016. Retrieved at https://www.rmf.harvard.edu/cbsreport

