4 min read
How to Reduce the Risk of Harm from Medication Errors in Children
Performance Health Partners
July 31, 2023

Reducing the risk of harm from medication errors in children – one of the most common types of medical error – is crucial for their safety and well-being. According to industry experts, medication errors are a significant source of preventable adverse events, carrying the potential to cause a higher rate of harm in children than in adults. Research shows that children are thrice as likely to experience a potential adverse drug event compared to adults. Read on to learn strategies to mitigate the risk of harm from these errors.
The Centers for Disease Control and Prevention reports a startling number of approximately 150,000 pediatric emergency department visits each year related to adverse drug events. This is further underscored by studies that estimate nearly 7.5 million preventable medication errors annually involve pediatric patients in the United States, of which 14-31% could potentially result in severe harm or even death.
The risks for medication error escalate during patient transitions between care, specifically when moving from inpatient to outpatient settings. As per the data from The American Journal of Managed Care, there is at least one medication error during hospital discharge for 26-33% of pediatric patients.
Underlying Causes of Medication Errors in Children
There are a variety of factors that contribute to the occurrence of medication errors in children:
- Weight-Based Dosing: Medications for children are often prescribed based on their weight, and miscalculations or misinterpretations of weight can lead to dosing errors.
- Lack of Pediatric-Specific Information: Many medications used in children have limited pediatric-specific dosing information available. Healthcare providers may need to adapt adult dosages or rely on their clinical judgment, which can increase the risk of errors. For instance, between August and December 2022, Canada was grappling with severe medication shortages. Because of the shortage, parents were opting to give their children what they believed were the correct dosages of adult medication. Consequently, the Ontario Poison Centre reported a surge in calls concerning unintentional dosing errors with acetaminophen and ibuprofen. The increase was considerable, ranging between 40% and 60% more than the previous four years.
- Complexity of Medication Regimens: Children with chronic conditions or complex medical needs may have multiple medications to manage. The complexity of these regimens, including different dosages and administration schedules, increases the likelihood of errors.
- Communication Issues: Misunderstandings and errors often stem from poor communication between healthcare providers, parents, and caregivers. Problems arise when the exchange of crucial information about medication history, dosages, and instructions is incomplete or inaccurate, contributing to potential medication errors.
- Distractions and Interruptions: The hustle and bustle of healthcare settings, particularly in hospitals, can increase the risk of distractions and interruptions during medication administration, thereby increasing the likelihood of errors. Healthcare providers working in high-stress environments with heavy workloads may face time pressures, which can also increase the likelihood of errors.
- Confusion Over Similar Medications: Medications with similar names or packaging can often cause confusion, leading to medication errors. This typically happens during the prescribing and dispensing phases, where look-alike or sound-alike drugs can easily be mistaken for one another.
- Lack of Pediatric Training and Knowledge: Healthcare providers who lack sufficient pediatric-specific training and experience may be less familiar with pediatric medications, leading to prescribing or dosing errors.
- Medication Administration Challenges: Dispensing medications to children, particularly infants and young toddlers, often presents considerable challenges. Issues like accurately measuring liquid medications or persuading a child to consume the medication can inadvertently lead to errors.
- System and Process Issues: Inadequate systems and processes for medication prescribing, dispensing, and administration, such as lack of electronic prescribing systems or barcode scanning, can increase the likelihood of medication errors.
Common Types of Medication Errors in Children
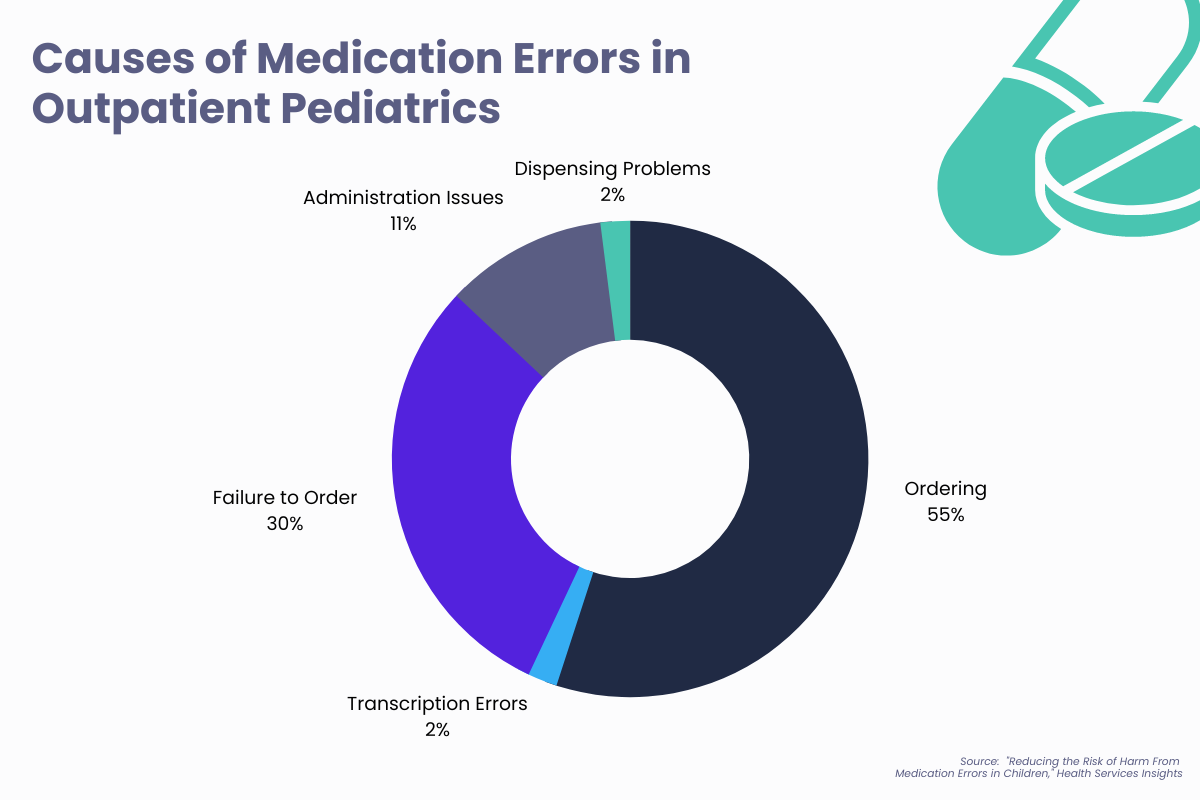
Research published in “Health Services Insights” illustrated that among 147 reported medical errors across 14 pediatric practices, 47 of the errors were medication errors. Of these, 55% were related to ordering, 30% were due to failure to order, 11% resulted from administration issues, 2% were transcription errors, and 2% involved dispensing problems.
The types of medication errors that are most prevalent in pediatrics include but are not limited to the following:
- Incorrect Dosing: One of the most prevalent medication errors in children involves inaccurate dosing, which could result in under or overdosing.
- Wrong Medication: Administration of the incorrect medication to a child is another significant error. It can happen due to similarities in drug names or packaging, look-alike/sound-alike medications, or mix-ups during medication preparation or administration.
- Administration Errors: Errors during medication administration may include incorrect administration routes, timing, or usage of improper technique or device.
- Medication Omissions: Medication omissions involve missing doses or failing to administer prescribed medications to children. These types of errors can occur due to miscommunication, lack of awareness, or oversight during medication administration.
- Prescribing Errors: Errors in prescription like incorrect dosage instructions, incorrect frequency or duration, or illegible prescriptions can lead to medication errors.
- Wrong Strength or Formulation: Administering medication with the incorrect strength or formulation can result in dosing errors and potential harm to the child.
- Drug-Drug Interactions: Children who take multiple medications, including prescription drugs and over-the-counter medications, are at risk of drug-drug interactions. These interactions can lead to adverse effects or reduced efficacy of medications.
Proactive Measures to Reduce Risk of Pediatric Medication Errors
Healthcare organizations play a vital role in reducing the risk of harm from medication errors in children. Some strategies that organization can implement are:
- Standardized Pediatric Guidelines: Develop and implement guidelines and protocols tailored specifically to pediatric patients for medication prescribing, dosing, administration, and monitoring. These guidelines should account for age-appropriate dosing and safety considerations.
- Medication Safety Programs: Establish comprehensive medication safety programs that focus on the prevention, detection, and mitigation of medication errors in pediatric settings. These programs should include regular training, education, and communication initiatives for healthcare providers. Provide ongoing training and education to healthcare providers regarding pediatric medication safety. This includes topics such as age-appropriate dosing, weight-based calculations, recognition of common medication errors, and effective communication with pediatric patients and their families.
- Technology Integration: Utilize technology solutions to enhance medication safety. This may include electronic prescribing systems, computerized physician order entry, barcode scanning, electronic medication administration record systems, and incident reporting software. These technologies can help reduce medication errors related to handwriting, dosing calculations, and improve medication tracking and reconciliation.
- Medication Reconciliation: Implement robust medication reconciliation processes to ensure accurate and up-to-date medication lists for each child. This involves comparing the medications the child is currently taking with newly prescribed medications to identify and resolve any discrepancies or potential interactions.
- Reporting and Learning Systems: Establish a culture of reporting and learning from medication errors. Encourage healthcare providers to report errors and near misses without fear of punitive actions. Analyze reported incidents, identify root causes, and implement strategies to prevent similar errors from happening in the future.
- Patient and Family Engagement: Involve patients and families in medication management, providing them with understandable information about medications, dosages, administration techniques, and potential side effects.
- Quality Improvement Initiatives: Conduct regular audits, performance reviews, and quality improvement initiatives to identify areas for improvement and implement strategies to reduce medication errors. Monitor medication-related indicators and outcomes to track progress and make evidence-based changes. Promote research and the adoption of evidence-based practices in pediatric medication safety. Stay current on the latest research, guidelines, and best practices to continuously improve medication safety processes.
By implementing these strategies, healthcare organizations can create a culture of safety, enhance communication and collaboration, and reduce the risk of harm from medication errors in children.
Ready to learn more?
Want to learn more about how an incident management system can prevent medication errors in children and improve patient outcomes at your organization? Request a free demo with our team.


