Near miss events are far more common than adverse events and typically occur many times before a harmful incident happens. Although near miss events can be viewed as learning and safety improvement opportunities, preventing them in the first place will ensure optimal patient safety and quality care. Read on to learn more about how to avoid near miss events in healthcare.
What Is a Near Miss?
A near miss (also known as a "close call" or "good catch") is a hazard or incident that might have resulted in harm but the problem did not reach the patient because of timely intervention by healthcare providers, the patient, or the patient’s family.
One example of a near miss: a high-risk patient needs to ambulate to maintain his strength while on bed rest. However, the non-skid socks the patient is supposed to wear are left behind in his room as he takes a walk around the unit. A staff member notices the socks and notifies a supervisor to prevent patient injury. There is no harm that results from this incident.
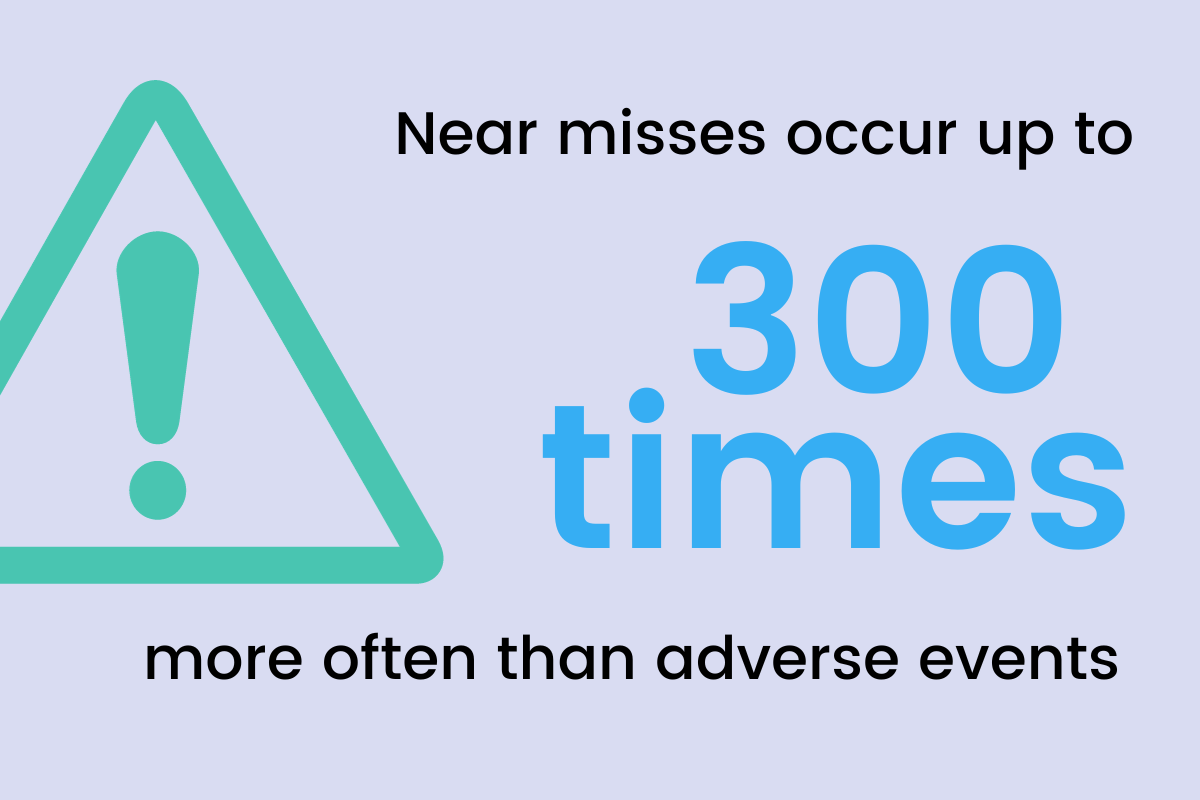
Experts estimate that near misses like this one occur up to 300 times more often than adverse events – events that cause harm to a patient as a result of medical care – in healthcare settings. Furthermore, they typically happen multiple times before the occurrence of a related adverse event. A 2023 study by the National Institutes of Health (NIH) found that near-miss events occur in nearly 23% of emergency department cases.
As a result, near miss events are often seen as learning and improvement opportunities within organizations that foster a culture of safety. These organizations might consider how a near miss event will put other patients at risk. They acknowledge the near miss event, value feedback, and make appropriate improvements rather than mistakenly assume the care setting is safe because a harmful event did not occur.
Barriers to Near Miss Reporting in Healthcare
Despite the opportunity reporting near misses in healthcare provides for safety improvement, they are underreported in healthcare for several reasons. Some barriers to near miss reporting include:
- Guilt or fear of punishment: Historically, a culture of blame and a fear of reprimand – including potential job loss or the loss of license – have been among the most influential reasons staff avoid reporting near misses and other incidents.
- Limited time to report: Fast-paced work environments and higher than optimal workloads prevent providers from having the time to report the critical details of an incident while they are top of mind.
- Lack of trust in follow-up: In organizations with inadequate reporting processes, providers are often frustrated when they repeatedly report incidents, but do not hear back from the administration and remain in the dark about what – if any – actions have been taken regarding reports.
- Limited incident reporting system: As healthcare providers administer care in more varied types of healthcare settings, safety and quality improvement tools like incident reporting software must adapt. But many reporting tools used by healthcare organizations are antiquated, time consuming, and not accessible to all employees.
For these reasons and more, the underreporting of near miss events and other types of incidents have left healthcare organizations with limited access to valuable data that could allow them to avoid near miss events and other types of incidents from happening in the first place.
How to Avoid Near Miss Events in Healthcare
The root causes of near miss events and adverse events are similar. As a result, identifying the root causes of these types of safety events in healthcare is key to correcting them and preventing them from happening in the future.
One of the best ways to avoid near misses in healthcare is by implementing an incident reporting system, which can collect and analyze a variety of data to detect the root causes of events, and thus provide opportunities for intervention.
Reporting near miss events using an incident reporting system helps to:
- Reduce risks for all patients by not waiting for harm to occur
- Prompt improvements in weak spots in the processes of care
- Notify providers to possible vulnerabilities and gaps in training
- Contribute to planning, recovery testing, and harm mitigation strategies
When selecting an incident reporting system, it’s important to look for one that:
- Is dynamic enough to easily capture all incidents, but is also user-friendly
- Is customizable to the specific needs of an organization
- Focuses on outcomes
- Can define measures and processes that will achieve the best possible operational, financial, and clinical results
- Supports comprehensive follow-up processes
Once an incident reporting system has been employed, all relevant stakeholders should be encouraged to utilize it to maximize its benefits. Below are a few tips on how to increase reporting frequency, and thus get your workforce to fully embrace a culture of safety.
- Launch a good catch campaign. A good catch campaign (or near miss program) is an incentive-based program that fosters a culture of safety by training, encouraging, and recognizing staff for identifying and reporting risk before it harms a patient. These campaigns help to encourage near miss reporting while defining gaps in system processes.
- Keep leadership engaged. When you keep data associated with near miss event reporting in front of the C-suite, the numbers become hard to ignore. Staff respond when they see leadership embracing a safety of culture as well as opportunities to expose vulnerabilities and make improvements.
- Educate and encourage staff. Staff need to be assured that reporting a near miss does not mean someone will be punished. They should feel comfortable coming forward to share lessons learned to prevent recurrence and understand that you can’t fix what you don’t know is broken.
- Keep communication open. Bringing staff into the conversation, listening to what they say, and acting on their expertise is empowering for all involved. Keeping progress reports in front of staff and drawing attention to how their work has created change motivates them to continue working toward safety goals. Rewards and incentives provide encouragement, but consistent communication is the greater motivator.
When your workforce sees that action plans are fully implemented and effective, they are more likely to report near miss events and other incidents, participate in the RCA process, and change their perception of the patient safety culture, decreasing near miss events and bringing the organization closer to zero harm.


