4 min read
Improving Patient Safety: How to Tackle Inaccurate Medication Lists
Performance Health Partners
April 3, 2023

Medication errors can have serious consequences for patients, including hospitalizations, longer stays, and even death. One common cause of medication errors is inaccurate medication lists. Patients may have multiple healthcare providers, and their medication lists may not be consistently updated or accurately recorded. In this blog post, we will explore how incident reporting can prevent medication errors resulting from inaccurate medication lists.
Maintaining an accurate patient medication list is essential for providing safe and effective healthcare. There are a variety of changes that can be implemented across an organization to prevent inaccurate patient medication lists.
Culture, Leadership, and Governance
Standardizing the medication reconciliation process is crucial for ensuring patient safety, meeting regulatory and accreditation requirements, and improving operational efficiency. Rushed or inaccurate medication histories can have serious consequences for patients.
Make sure to identify and address organizational factors such as shortened appointment times and incomplete medication lists. Recognizing and celebrating “good catches” can be an effective way to promote a culture of patient safety and encourage staff to be vigilant in identifying medication reconciliation errors.
Patient and Family Engagement
Include the reason for taking the medication on the home medication list and throughout all documentation systems to ensure that healthcare providers have a complete understating of the medication orders, care planning, and discharge planning.
Engaging patients in the medication reconciliation process is crucial for ensuring accuracy and completeness of their medication lists. Patient navigators can play a crucial role in educating patients on the use of portals and encouraging their use to double-check current medication lists.
Learning System
Developing a flowchart of current processes can be a useful tool for identifying areas where medication reconciliation processes can be streamlined and improved. The chart can highlight unnecessary steps and define roles and responsibilities.
Sharing post-implementation audit findings is essential for driving continuous improvement activities and ensuring that medication reconciliation processes remain effective over time. These findings can include items such as staff-related knowledge deficits and barriers to staff engagement with the process.
Conducting multidisciplinary training sessions and identifying medication reconciliation coaches can be effective ways to ensure that staff are trained and confident in their ability to perform medication reconciliation accurately and effectively.
Workforce Safety
Having a distraction-free environment during the intake or admission process is essential to ensure staff can collect and document a patient's medication information accurately and thoroughly. Ensure that a culture of high reliability is nurtured so staff are sensitive to operations and feel safe to report system issues that can lead to medication reconciliation errors. With encouraging staff to report, it is also important to have a proper and easy to use incident reporting software in place.
Incident reporting software allows healthcare providers to document and report incidents and near misses that occur in the delivery of patient care. Incident reports provide a mechanism for identifying areas of concern and implementing interventions to prevent future errors.
Examples of Medication Errors Prevented by Incident Reporting
Incident reporting software can also be used to document medication errors resulting from inaccurate medication lists.
Inconsistent knowledge and record keeping about medications cause up to 50% of medication errors in hospitals and up to 20% of adverse drug events.
By reporting these incidents, healthcare providers can identify patterns and trends in medication errors, such as specific medications or patient populations that are at higher risk. This information can be used to develop targeted interventions to prevent future errors.
Duplicate Medications
One common medication error resulting from inaccurate medication lists is the prescribing of duplicate medications. Patients may see multiple healthcare providers who prescribe medications for the same condition, leading to duplicate medications.
In a study done involving 94 voided medication order errors, it was found that almost half of the errors were related to duplicate orders. This can increase the risk of adverse drug reactions and other complications.
Through incident reporting, healthcare providers can identify patients with duplicate medications and work to reconcile their medication lists. This may involve communicating with other healthcare providers or reviewing pharmacy records to ensure that the patient's medications are accurate and up-to-date.
Omitted Medications
Another medication error that can result from inaccurate medication lists is the omission of necessary medications. Patients may not remember all of their medications or may not disclose all of their medications to their healthcare provider. This can lead to important medications being left off of the patient's medication list.
Medication reconciliation errors at hospital admission are noted in 36% of patients and occur mostly during the medication history gathering phase
Incident reporting can help identify patients who have been prescribed medications that are not included on their medication list. This can prompt healthcare providers to review the patient's medication history and reconcile their medication list to ensure that all necessary medications are included.
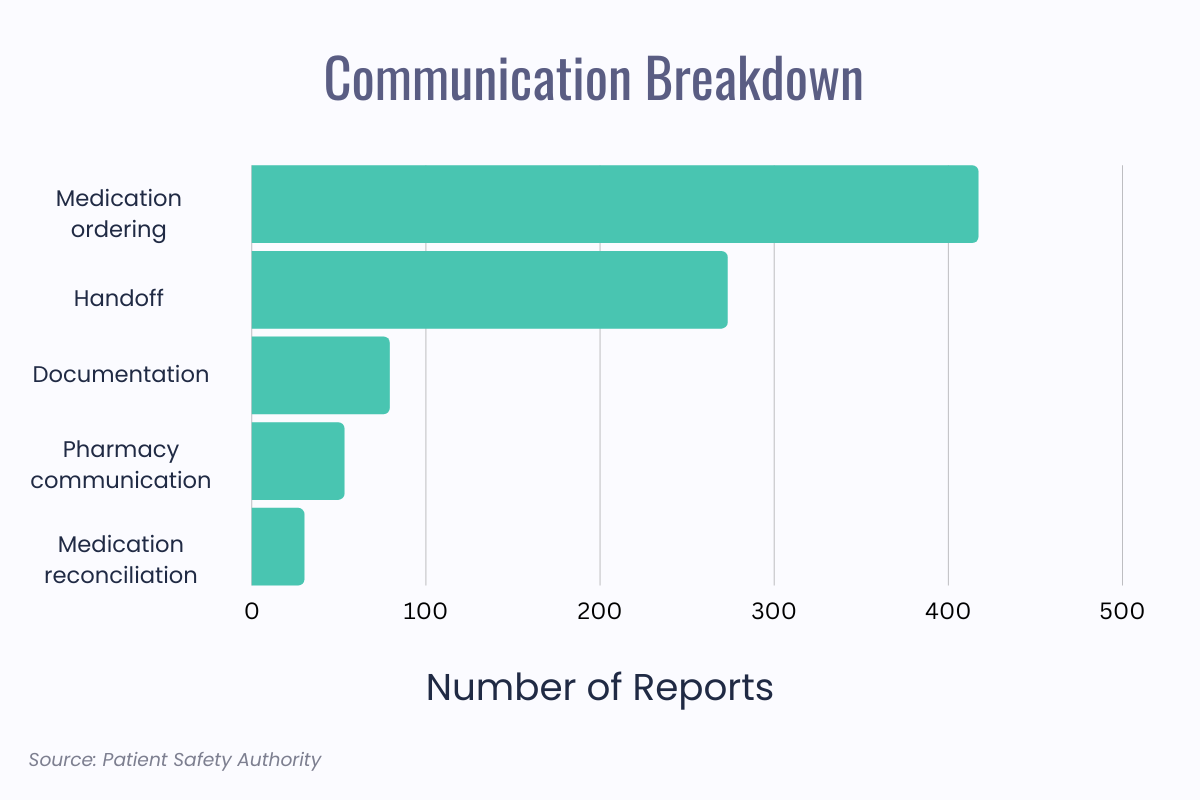
A study completed in 2018 using reports from the PA-PSRS database found the communication breakdowns were an issue in 75% of all reports. With an incident reporting software in place, these breakdowns can be caught early and it will be easier for management to see which part of the medication administration process is having the most communication issues. Seeing this data will allow them to implement processes to help avoid the breakdowns from occurring again.
Incorrect Dosages
Inaccurate medication lists can also lead to incorrect dosages of medications being prescribed or administered.
Patients may have changed their medication regimen without informing their healthcare provider, leading to discrepancies in the medication list. This can result in patients receiving incorrect dosages of medications, which can have serious consequences.
Up to 91% of medication reconciliation errors are clinically significant and 1% to 2% are serious or potentially life-threatening.
Incident reporting can help identify patients who have been prescribed incorrect dosages of medications. This can prompt healthcare providers to review the patient's medication history and reconcile their medication list to ensure that the correct dosages are being prescribed and administered.
Adverse Drug Reactions
Finally, inaccurate medication lists can increase the risk of adverse drug reactions. Patients may be prescribed medications that interact with other medications they are taking, leading to adverse drug reactions. If these medications are not accurately recorded on the patient's medication list, healthcare providers may not be aware of the potential for adverse drug reactions.
A study conducted in 2019 revealed nearly 41% of hospital discharge patients had at least one medication discrepancy resulting in a potential for an adverse drug events.
Incident Reporting Software to Prevent Medication Errors
Incident reporting can help identify patients who have experienced adverse drug reactions as a result of inaccurate medication lists. This can prompt healthcare providers to review the patient's medication history and reconcile their medication list to ensure that potential drug interactions are identified and addressed.
Inaccurate medication lists can have serious consequences for patients, including medication errors, hospitalizations, and adverse drug reactions. Incident reporting software can be a powerful tool in preventing medication errors resulting from inaccurate medication lists.
By documenting and reporting medication errors, healthcare providers can identify areas of concern and implement targeted interventions to prevent future errors. Ultimately, incident reporting can help improve patient safety and reduce the risk of medication errors.
Want to learn more about how an incident management system can improve patient safety and outcomes at your organization? Request a free demo with our team.


