A root cause analysis (RCA) is an essential tool in healthcare for reevaluating systemic issues and implementing significant improvements for better patient outcomes. Knowing the correct approach to performing a root cause analysis is crucial for enhancing an organization’s problem-solving capabilities and ensuring long-term success. Continue reading to learn how to perform a root cause analysis in your own organization.
What is a Root Cause Analysis?
In healthcare, root cause analysis serves as a methodical tool to examine significant adverse events. The primary objective of an RCA is to uncover potential issues within processes that elevate the risk of errors while remaining non-punitive.
A successful RCA can pinpoint contributing factors to adverse events, enabling the implementation of measures to:
- Improve patient safety
- Prevent similar safety events from happening again in the future
- Reduce associated risk-related costs
RCA methodologies systematically identify failures or issues within a system, shedding light on areas for improvement and guiding the development of effective preventive measures.
Whether an incident raises concerns about liability or questions the practices of an employee, it’s crucial to emphasize that an RCA must be conducted as a distinct process independent of an employee’s performance review.
The primary emphasis during RCA should be on evaluating entire systems rather than singling out individual employee performance. This separation ensures a more comprehensive understanding of the factors contributing to incidents and facilitates the development of systemic improvements.
How to Identify When an RCA is Needed
A wide spectrum of issues may prompt the need for an RCA, spanning from specific and tangible concerns like medication errors or in-patient falls to broader systemic challenges such as high readmission rates and compliance issues. Events and issues can come from many sources (e.g., incident reports, risk management referrals, resident or family complaints, health department citations, etc.).
It’s important to emphasize that the creation of a secure and supportive atmosphere for incident reporting is crucial to kickstart a comprehensive root cause analysis and is the first step in how to perform a root cause analysis. Incident reporting is a trigger for initiating an RCA, and fostering a non-punitive culture of safety encourages more frequent reporting of incidents.
In healthcare, a sentinel event refers to: a patient safety event that reaches a patient and results in death or serious physical or psychological injury.
Sentinel events demand immediate attention and thorough investigation to prevent recurrence. An RCA should be performed after each sentinel event to identify underlying causes and implement preventive measures effectively.
The National Patient Safety Foundation (NPSF) released a report titled “RCA2: Improving Root Cause Analyses and Actions to Prevent Harm,” which emphasized the importance of corrective actions and resultant risk mitigation and outlined nine formal recommendations to improve the RCA process. The nine formal recommendations include:
- Leadership Involvement: Leadership must actively support the RCA2 process, ensuring thorough reviews and acting when needed.
- Regular Process Evaluation: Leadership should annually review the effectiveness of the RCA2 process for continuous improvement.
- Define Non-RCA Events: Clearly outline events unsuitable for RCA2 review to focus efforts on relevant incidents.
- Prioritize Reviews: Establish a transparent risk-based prioritization system to identify events requiring RCA2 review.
- Swift Initiatives: Initiate RCA2 reviews within 72 hours of recognizing the need, emphasizing prompt action.
- Expert Teams: Compose RCA2 teams with diverse expertise, including process experts and a patient representative unrelated to the event.
- Allocate Investigation Time: Provide dedicated work hours for staff on RCA2 teams to conduct thorough investigations.
- Utilize Appropriate Tools: Equip teams with effective RCA2 tools, such as Flow Diagramming and Cause and Effect Diagramming, to identify corrective actions.
- Offer Feedback: Share RCA2 findings with staff, patients, and their families to promote transparency and continuous improvement in patient safety.
Key Steps in Performing an RCA
Step 1: Assemble a Multidisciplinary Team
The role of a leader in an RCA team in healthcare involves:
- Assembling and managing the team
- Guiding the analysis
- Documenting and reporting findings to the appropriate people
It’s imperative that the team leader is appointed by leadership and has the appropriate background to oversee an RCA. Team members are people with personal knowledge of the processes and systems involved in the event that is being investigated.
Step 2: Data-Collection
The next step in how to perform a root cause analysis is data collection.
In this step, the RCA team will gather relevant information and evidence surrounding the incident to understand what happened and create a preliminary timeline. It’s important to utilize all potential data sources including interviews, observations, and document reviews.
Once all information is collected, the team should draft a timeline and come to a consensus about the sequence of events to avoid any inconsistencies or missing information.
Step 3: Identify the Root Cause
Every incident has a direct cause, which is the immediate occurrence or condition that caused the incident; however, a direct cause is not a root cause.
A root cause is a fundamental, underlying issue within processes or systems that contribute to the occurrence of a harmful event. Often, multiple root causes can be identified for a single event.
Step 4: Perform Analysis
When considering how to perform a root cause analysis, organizations have a broad spectrum of RCA methodologies to choose from:
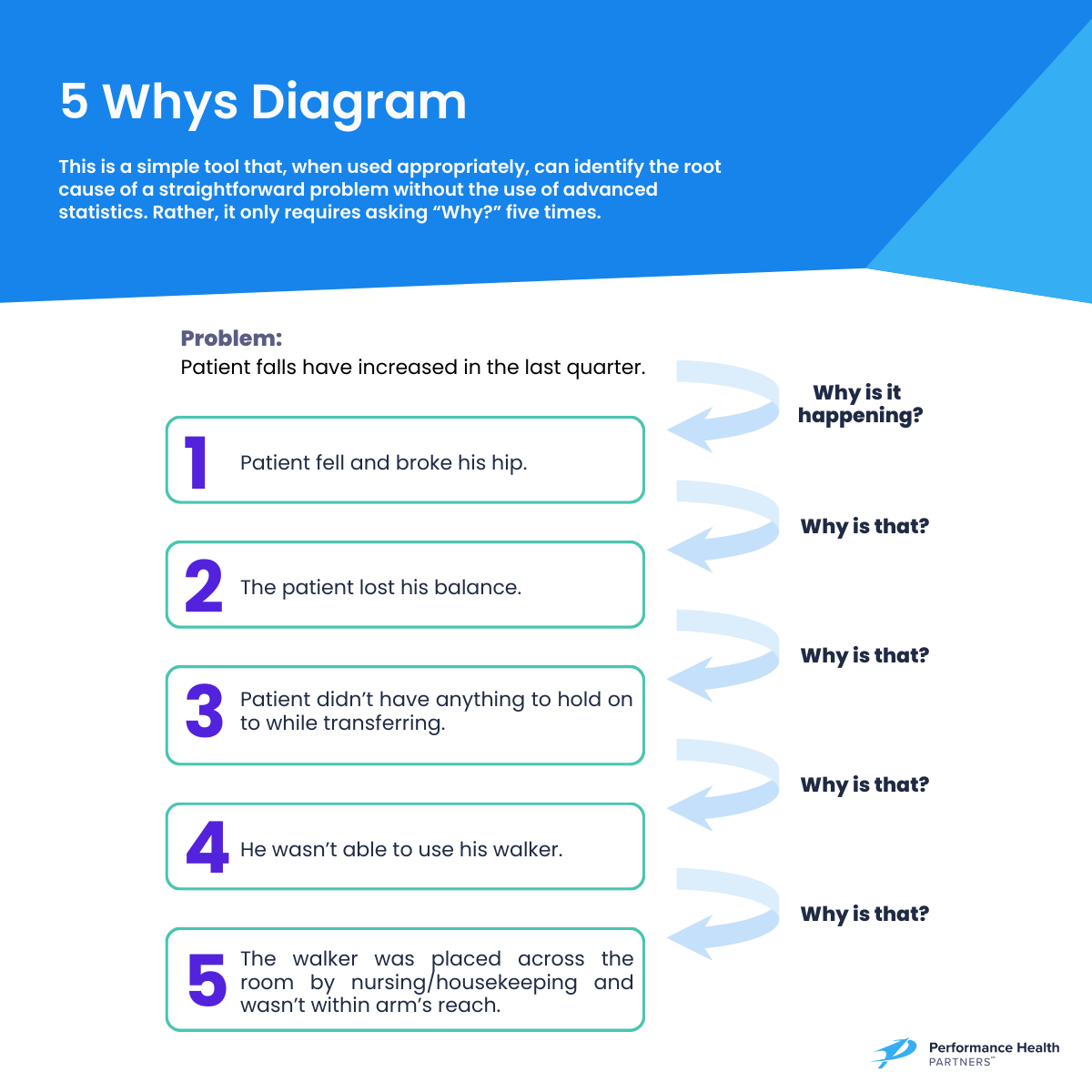
- The 5 Whys method uses iterative questioning and stands out as an easy-to-implement, beginner-friendly approach suitable for straightforward problems without requiring advanced statistics.
- Another introductory method is the Fishbone diagram, using visual categorization of root causes, which allows for visual analysis and prioritization of causes for action, making it a preferred option for some organizations.
- For more complex analyses, Failure Mode and Effects Analysis identifies faulty process parts and assesses interventions, applicable not only in RCA but also for reviewing new
- The Pareto Chart adds a layer of analysis by incorporating the significance of problems by frequency or cost.
- The RCA2 method, developed by the National Patient Safety Foundation, is often regarded as the most comprehensive guide for efficient and effective RCAs. However, given the significant resources and commitment it demands, this method is best suited for institutions with robust capabilities.
Step 5: Develop Actionable Recommendations
In this next phase, once the team has pinpointed the root causes, their focus shifts to creating actions aimed at mitigating or preventing these causes from leading to further harmful events. These changes can include adjusting current processes or creating entirely new procedures.
Keep in mind that the objective is to find actions that make substantial changes while also being sustainable for the organization to implement and maintain. Involvement of leadership is crucial in this stage, given that certain actions may necessitate a comprehensive understanding of diverse patient care systems and the facility’s resource allocation priorities.
When developing corrective actions, consider questions such as:
- What safeguards are needed to prevent this root cause?
- How do we avoid contributing factors triggering its reoccurrence?
- Can procedural changes ensure this root cause never happens?
- If a similar event occurs, how do we swiftly prevent harm to the patient?
- How can we minimize the impact on the patient if harm arises from this root cause?
Step 6: Implementation
Once corrective actions have been identified, the RCA team should establish a timeline for implementing the plan, considering resource allocation.
To retrospectively evaluate the success of the RCA, it is crucial to identify indicators of success during this period, such as a reduction in medication errors or the closure of compliance gaps. This helps gauge the effectiveness of the healthcare root cause analysis and determines whether further analysis is necessary. Delegating the evaluation of a specific RCA plan should occur before disbanding the RCA team.
Tips and Best Practices
While RCA can be a valuable tool for enhancing organizational standards and patient safety when used effectively, common pitfalls may render it ineffective in resolving problems and may result in missed opportunities for improvement.
To ensure an effective RCA:
- Don’t jump to conclusions. As stated previously in the data-collection section, it is important to get a full, comprehensive view of the incident and contributing factors before analyzing and identifying a root cause. It can feel tempting to jump to conclusions due to time constraints or already-known issues, but this can lead to failure in preventing a future incident.
- Consider human factors. When concluding, consider biases, drift, and cultural influences. Human factors such as cognitive biases, normalization of deviance (drift), and organizational culture can significantly impact incident causation and should be thoroughly examined to develop robust preventive measures.
- Don’t focus on individuals. RCAs can often bring up feelings of judgment among team members. Therefore, it’s important for leadership to reiterate the importance of taking an objective, non-judgmental outlook during an RCA.
- Don’t just address the symptoms. Address the cause. For effective RCA, the action plan must address the root cause, not just surface-level issues. Solving only immediate problems neglects deeper, systemic issues that may cause future harm.
Ready to Get Started?
Learn how Performance Health Partners’ industry leading healthcare safety software can help your organization streamline the root cause analysis process and improve patient safety. Click here to get started.



